Going vegan may help prevent diabetes in overweight people
Diabetes

"Going vegan can prevent overweight adults from developing type 2 diabetes, an 'important' new study has concluded," reports the Mail Online.
"Going vegan can prevent overweight adults from developing type 2 diabetes, an 'important' new study has concluded," reports the Mail Online. Researchers in the US investigated the effects of a 16-week vegan diet on a group of overweight people compared with a group that continued their usual diet.
The vegan group showed improvements in beta-cell function. Beta cells play a key role in regulating blood insulin levels, and deterioration in their function is often associated with the gradual onset of type 2 diabetes. People in the vegan group also had a reduction in body mass index (BMI) and fat levels compared with the usual-diet group.
Vegan diets tend to have less fat and sugar than a conventional Western diet, and reducing fat and sugar intake is known to reduce diabetes risk, so the results are not particularly surprising. The challenge is getting people to stick to these diets or, for those who don't want to go vegan, a similar balanced diet that contains fish and low-fat dairy products.
This study mainly involved women who were health-conscious, which means they may be more likely to adhere to dietary restrictions. Repeating the experiment with groups from different backgrounds would help determine how successful it may be in larger populations.
For people with a confirmed diagnosis of type 2 diabetes, a diet-only approach may not be enough to control blood sugar levels.
Where did the story come from?
The study was led by researchers from the Physicians Committee for Responsible Medicine (PCRM) in Washington DC, and researchers from 4 other international institutions in the Czech Republic, Italy and the US.
It was funded by the PCRM and published in the peer-reviewed medical journal Nutrients on an open-access basis, so it's free to read online.
While the Mail Online largely reported the story accurately, it was somewhat over-optimistic about the results – the study was too small and too short to show that a vegan diet prevents diabetes. Also, none of the participants, in either group, had diabetes by the end of the trial.
What kind of research was this?
This was a randomised controlled trial where one group was asked to follow a low-fat vegan diet and the other to carry on eating as normal. Randomised controlled trials are the most reliable way of assessing the effect of an intervention, but their power depends on good randomisation to balance confounders, a large sample size and making the effort to follow up the participants.
What did the research involve?
The researchers recruited overweight men and women aged 25 to 75 years with a BMI of between 28 and 40. In adults, a BMI of 25 to 30 is classed as being overweight, and 30 or above as obese. People who had diabetes, smoked, abused alcohol or drugs, were pregnant or were currently eating a vegan diet were excluded.
A total of 75 people took part in the study – 38 in the intervention group and 37 in the control group – 96% of whom completed the study.
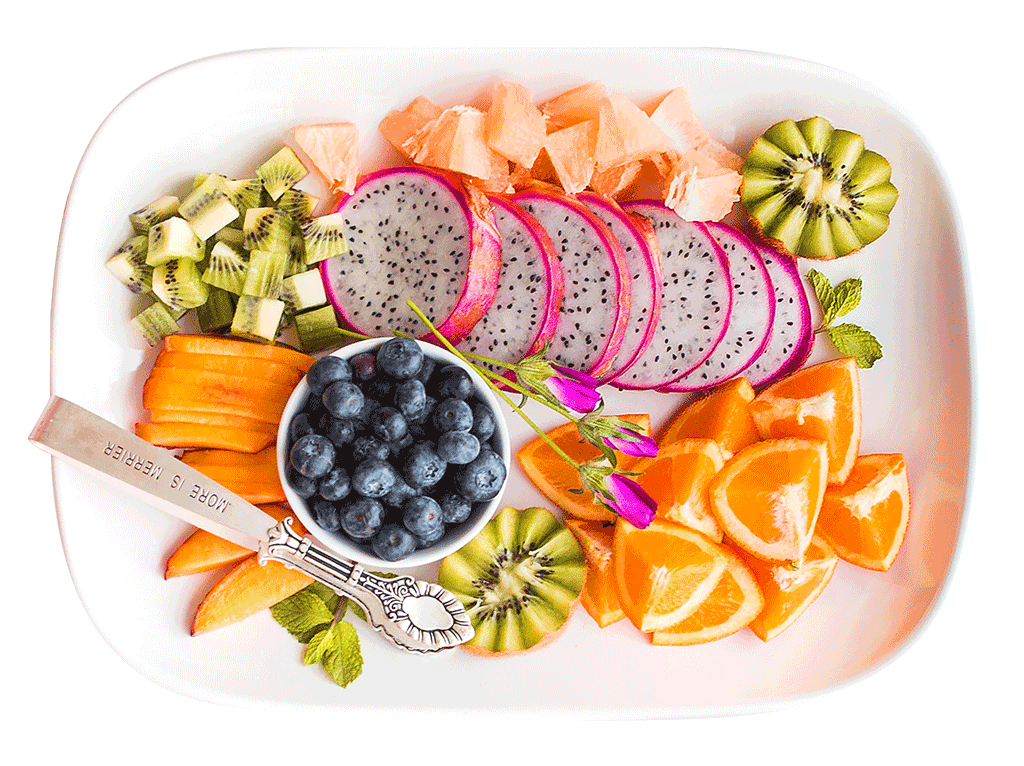
Participants were randomly assigned to the intervention or control group. The former were asked to follow a low-fat vegan diet consisting of vegetables, grains, legumes, fruits and carbohydrates. No meals were provided, so participants had to make all meals themselves. The control group were asked to make no meal changes. In both groups, alcoholic drinks were limited to 1 a day for women and 2 a day for men.
All participants were asked to complete a 3-day food diary at baseline and 16 weeks. Dietitians analysed this data and made unscheduled telephone calls to participants to assess dietary adherence.
They were also told not to change their exercise habits – measured using the International Physical Activity Questionnaire, a well-validated assessment system for physical activity – and asked to keep taking any prescription medicine as normal.
At the end of the study, the researchers tested whether there were any correlations between beginning the vegan diet and changes in:
- beta-cell function – the ability of beta cells to store and release insulin
- insulin resistance – a measurement of how well cells respond to insulin
- visceral fat – fat that is deeper in the body or wrapped around the organs
- BMI
What were the basic results?
In the intervention group after 16 weeks:
- beta-cell function appeared to improve – lower levels of insulin were secreted between meals and greater levels secreted in response to meals
- fasting insulin resistance fell (-1.0, 95% confidence interval [CI] -1.2 to -0.8) – this was related to a reduction in BMI and loss of visceral fat
- BMI decreased by 2 (the average fell from 33.1 to 31.2) but barely changed in the control group (33.6 to 33.4)
- visceral fat volume decreased from an average of 1,289cm3 to 1,090cm3 but increased in the control group from 1,434cm3 to 1,459cm3
How did the researchers interpret the results?
They said beta-cell function and insulin sensitivity were significantly improved through a low-fat, plant-based diet in overweight adults using a 16-week intervention, adding: "Our study suggests the potential of a low-fat, plant-based diet in diabetes prevention."
Conclusion
This study showed that overweight individuals without diabetes who followed a vegan diet with no limit on energy intake can improve function of beta cells and fasting insulin resistance.
The study's strength lies in its method. It was a randomised trial, which is the best way to assess the effectiveness of an intervention. However, there were limitations:
- participants prepared their own meals, meaning any fluctuations to the diet plan were not controlled or recorded
- dietary intake relied on self-reporting, which has well-known limitations, such as participants not remembering what they ate or not being honest if they went off-plan
- most of the participants were already health-conscious, so they may have been more likely to stick to a vegan diet and are not representative of the whole population
- the sample size was small – the experiment would need to be repeated in larger and more diverse populations before any definitive conclusions could be drawn
Further research is also needed to see whether improvements in beta-cell function require a 100%-vegan diet or if the beneficial effects can be achieved with smaller changes.
Finally, it's important to note that non-vegan diets that include low-fat dairy products and oily fish, among other recommendations, can also aid weight loss and help control or prevent type 2 diabetes.
Read more advice about reducing your type 2 diabetes risk.






 Subscribe
Subscribe Ask the doctor
Ask the doctor Rate this article
Rate this article Find products
Find products